Functional Sensory symptoms describe sensory symptoms anywhere in the body that are due to the nervous system not working properly. They are not caused by damage or disease of the nervous system.
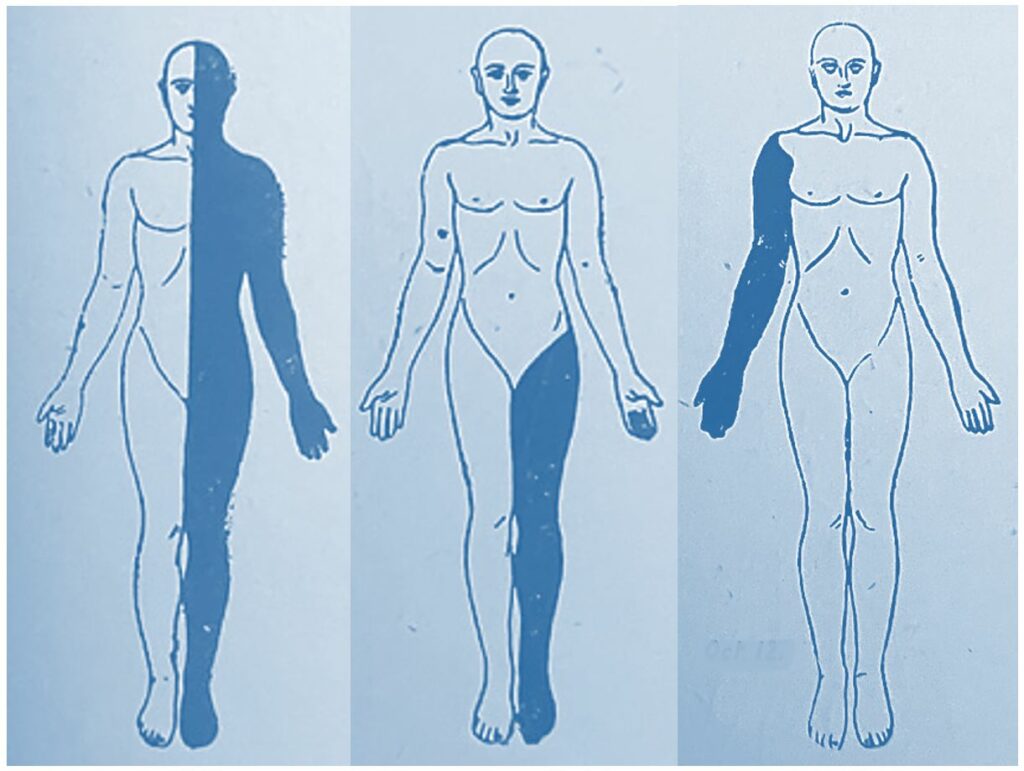
Patients with functional sensory symptoms can experience the following:
To the patient and the doctor, these symptoms can be alarming. They may make you wonder if you have had a stroke or multiple sclerosis.
However, functional sensory symptoms are not due to damage to the nervous system which means that they can get better or even go away completely. This is because when people have functional sensory symptoms all the parts of the nervous system are there, they are just not working properly so that your brain does not receive the messages in the normal way.
The diagnosis of functional sensory symptoms is usually made by a neurologist.
When the doctor listens to your story and examines you they may recognise your symptoms as typical of functional sensory symptoms. On examination the doctor may find that sensation in the affected area is reduced. There may be a mild degree of weakness in association with the sensory disturbance. The pattern of this weakness and response to specialised tests on examination will help the doctor make a positive diagnosis of your condition.
Normal scans and tests help to make the diagnosis, but the diagnosis is usually made by a neurologist when they first meet you.
Functional sensory symptoms arise for different reasons in different people. The reasons are very similar to those that cause functional weakness. These include


We will be re-directing you to the University of Edinburgh’s donate page, which enable donations in a secure manner on our behalf. We use donations for keeping the site running and further FND research.
