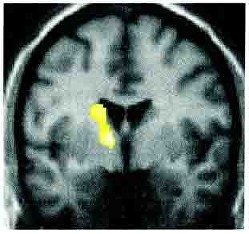
Изображение головного мозга показывает нам, как нервная система может неправильно функционировать у пациентов с функциональными симптомами. Эта фотография показывает однофотонную эмиссионную компьютерную томограмму пациента, страдающего функциональным парезом и нарушениями чувствительности на одной половине тела. Томограмма показывает, что при наличие этих симптомов в участке головного мозга с противоположной стороны нарушаются нормальные взаимодействия (что показано на рисунке желтым). Данный тип томографии показывает, что нервная система и функции головного мозга страдают при данных заболеваниях. Но это не означает, что Вы не можете ничего сделать, чтобы исправить это.
Фото от Vuilleimier et al. Brain 2001
Ответ прост: НЕТ!
Одна из серьезных проблем, с которой сталкиваются пациенты с функциональными и диссоциативными неврологическими симптомами – это ощущение, что им не верят. Частично это происходит от того, что многие доктора не обучены распознавать физические симптомы, не соответствующие какому-либо заболеванию, а исследования в этой области малочисленны. Некоторые врачи действительно не верят этим больным. Другие верят и пытаются помочь так, как если бы они помогали больным с органическим заболеванием (например, рассеянным склерозом). Итак, если это реальное сотояние, но не органическое болезнь, то вы спросите: “Что же это? У меня просто бурная фантазия и я всё это выдумал?“
Как мы уже ответили выше, «НЕТ!», вы не придумали и не просто изображаете симптомы, и, конечно же, «ВЫ НЕ СХОДИТЕ С УМА»! У вас имеются функциональные (диссоциативные) симптомы. Это состояние сложно осознать, и чтобы понять его, нужно время. У Вас нет поражения органа, но в тоже время ваши симптомы – это реальность, а не плод вашей бурной фантазии. Мы надеемся, что представленные ниже примеры, помогут вам понять это.
• Пример мигрени. Может помочь сравнить ваши симптомы с тем, что происходит при мигрени. Мигрень является распространенным состоянием, при котором все исследования головного мозга не выявляют патологии и которое может проявляться разнообразными неврологическими симптомами, такими как “вспышки света” перед глазами, покалывания на одной стороне тела или даже параличом. В отличие от функциональных расстройств, в отношении мигрени мы знаем несколько больше о том, какие отделы мозга работают неправильно и что патологически изменяется активность нейронов. Но тем не менее диагноз мигрени до сих пор ставится только лишь на основе рассказа пациента.
• Что происходит с человеком, когда он в гипнозе? Это “что-то в психике” или же это “измененное состояние мозга”? Многие люди восприимчивы к гипнозу. Все мы видели по телевизору, как люди под гипнозом не могли контролировать свои мысли и поведение. При этом, чтобы быть подверженным гипнозу, не обязательно иметь психические отклонения. Так что же, гипнотический транс – это измененное состояние мозга или психики? На оба вопроса можно ответить положительно, но, вероятно, наиболее правильно сказать, что вопросы поставлены некорректно. То же касается и пациентов с функциональными или диссоциативными симптомами, для которых нет смысла задаваться вопросом “Всё в моей психике?”. Поскольку и мозг и психика одинаково важны.
• Почему наличие депрессии при рассеянном склерозе считается вполне понятным? Многие пациенты с неврологическими заболеваниями становятся депрессивными или тревожными. Боль, инвалидизация, неопределенность будущего, проблемы с работой и семьей – всё это влияет на состояние человека. Особенно интересно, что многим пациентам с органическим диагнозом, как при рассеянном склерозе, обычно проще рассказать окружающим о плохом настроении и тревоге, потому что все знают о реальности их неврологического заболевания и относятся к ним с сочувствием.
Многие люди с функциональными симптомами НЕ ИМЕЮТ депрессии или тревоги. Но если депрессия и тревога есть, то им трудно рассказать об этом другим людям. Например, если у больного имеется функциональный парез с болью и утомляемостью, то есть несколько причин, почему он не желает рассказывать окружающим, что чувствует тревогу или подавленность:
Ответ на этот вопрос, несомненно (и к сожалению), «ДА», но сейчас это случается редко. В последнее время наблюдалось много случаев, когда люди пытались получить выгоду, симулируя болезнь, поэтому окружающие теперь относятся с недоверием к непонятным им симптомам. Например, человек, утверждавший, что он не может ходить, был заснят играющим в футбол. Другой видеоклип показал мужчину, который таскал тяжелые мусорные контейнеры, а между тем утверждал, что не может ничего поднимать. Был также случай, когда мужчина, пытавшийся получить компенсацию вследствие слепоты, был заснят превышающим скорость на шоссе. Когда такие пациенты симулируют симптомы во время обследования, они могут быть очень похожи на функциональные симптомы, однако имеются и существенные отличия. Как правило, симулянты рассказывают очень противоречивые истории (потому что они также выдуманы). Они описывают симптомы не так, как, действительно, страдающие от болезни люди. И, как правило, при детальном изучении жизни симулянта, всплывают факты судебных дел или других выгодах, получаемых от болезни (хотя, конечно, это не означает, что человек, переживающий судебные тяжбы не может тоже реально заболеть). Некоторые люди также предъявляют симптомы, чтобы попасть в больницу или добиться операции. Такие случаи называются “искусственно вызываемые (или артифициальные) расстройства” и встречаются также достаточно редко и по сути представляют собой расстройство поведения с преднамеренным нанесением вреда своему здоровью.
Таким образом, иногда люди демонстрируют симптомы, поэтому некоторые доктора (и пациенты) делают ужасную ошибку, полагая, что пациенты с функциональными симптомами «выдумывают» или «притворяются».
Некоторые пациенты с функциональными нарушениями обратили внимание, что их симптомы приходят и уходят странным образом, что иногда заставляет их задуматься, что, возможно, они сами «делают это». Это очень распространённое наблюдение, и вы должны понять, что они не способны сами «делать это».
Если вы нашли этот сайт, чтобы самостоятельно разобраться в своём состоянии, этот раздел очень важен для вас. Естественно, что пациенты не хотят иметь диагноз, который можно спутать с симуляцией. Мы уже говорили выше, что симуляция в настоящее время встречается весьма редко, но, тем не менее, некоторые врачи ошибаются в отношении пациентов с функциональными расстройствами и недостаточно серьёзно относятся к их симптомам. Чаще же доктора положительно относятся к вашим жалобам, но затрудняются их интерпретировать и понятно объяснить ваше состояние. Поэтому пациенты часто недовольны своими врачами, даже когда те им верят и пытаются помочь.
В течение многих лет, функциональные и диссоциативные неврологические симптомы назывались по-разному. Некоторые из них назывались “психиатрическими”, поскольку считалось, что все эти симптомы “от головы”. Психологические факторы часто достаточно важны в развитии функциональных расстройств, но это не означает, что симптомы придуманы. Большинство учёных убеждены, что эти симптомы существуют на границе между головным мозгом и психикой, между неврологией и психиатрией, вот почему сложно ответить, когда люди (и пациенты) спрашивают «это неврологическое или психическое заболевание?» Имеются доказательства как в пользу одного, так и другого. Хотя на самом деле данный вопрос не имеет смысла, потому что как наши движения, так и наши эмоции есть продукт работы мозга.
Ниже представленные термины могут быть сложны для понимания и не совсем приятны, но мы хотим помочь вам разобраться в них.
Конверсионное расстройство – этот термин был предложен Зигмундом Фрейдом и используется в стандартах американской классификации психических болезней (DSM-IV). Этот термин основан на теории, что пациент «конвертирует, переводит» свои психические проблемы в физические симптомы. Конверсионное расстройство проявляется параличами, нарушениями движений и чувствительности, неэпилептическими приступамию. Этот термин применим для небольшого количества больных, при этом нет достаточно экспериментальных данных, которые позволили бы применить его для описания большего количества больных (обычно, чем тяжелее симптомы, тем тяжелее была стрессовая ситуация). При следующем пересмотре классификации психических расстройств (DSM-V) этот термин заменен на расстройство функциональных неврологических симптомов, и наличие связи между психологическим стрессом и симптомами уже не требуется.
Диссоциативное расстройство – симптомы которого описаны в международной классификации болезней. Для получения большей информации откройте вкладку “Диссоциация”.
Неорганическое расстройство – это врачебный термин, используемый для симптомов при отсутствии очевидного органического заболевания. Это подразумевает, что проблема сугубо психологическая.
Психогенное расстройство – это термин, зачастую использовавшийся ранее для описания таких симптомов, особенно диссоциативных припадков и двигательных расстройств. Это также подразумевает, что проблема сугубо психологическая.
Психосоматическое расстройство – очень похож по значению на психогенное. Хотя суть этого термина в обратной связи между психикой и телом, т.е. тело влияет на состояние психики точно также, как состояние психики – на тело.
Расстройство соматизации – предполагает, что пациент имеет физические симптомы из-за психических проблем. Объяснения здесь такие же как и для «конверсионных расстройств». Расстройство соматизации наблюдается, когда в течение жизни человека имеются определенные физические симптомы, не связанные с органическими заболеваниями.
Истерия – это термин, который использовался около 2000 лет. Он означает «блуждающая матка» и появился в Древней Греции, где полагали, что женщины, страдающие физическими симптомами, имеют проблемы со своей маткой, которая «блуждает» по телу. В 18 и 19-х веках этим термином описывали все симптомы, не объясняющиеся другими болезнями. В 20 веке он стал применяться гораздо реже и только для определенного круга неврологических симптомов, а сейчас используется крайне редко.
Более чем в течение последних 100 лет пациенты с функциональными симптомами часто испытывали несправедливое отношение со стороны врачей. Традиционно, неврологи видели свою задачу при данных состояниях лишь в их диагностике, а на лечение пациентов отправляли к психиатрам.
В течение десятилетий многие неврологи негативно относилось к такого рода проблемам. И сейчас среди некоторых неврологов отмечается тенденция с подозрением рассматривать эти симптомы. Другие неврологи были бы готовы помочь, но не имеют соответствующих навыков. Отдельные неврологи делают необоснованные заключения о роли прошлых психиатрических или психотравмирующих проблем, что может быть непродуктивным. Сталкиваясь с такими ситуациями, пациенты постепенно теряют доверие и начинают сомневаться в диагнозе, установленном неврологом.
Большинство психиатров, исключая тех, которые работают в тесном контакте с неврологами, также ощущают неуверенность, сталкиваясь с функциональными и диссоциативными симптомами, и задаются вопросом, а не было ли пропущено неврологическое заболевание у пациентов с функциональными симптомами. На этой вкладке мы объяснили, насколько могут быть полезны психологи и психиатры в лечение функциональных расстройств, даже если у пациента нет депрессии или тревоги. Сотрудничающие с неврологами психиатры и медицинские психологи имеют специальную подготовку в данной области и обычно правильно понимают эти расстройства
Пациенты с функциональными жалобами, консультирующиеся у психиатров, часто ощущают, что врач расценивает симптомы как психические (“всё в голове”). Поэтому, естественно, многие пациенты предпочитают занять оборонительную позицию в общении с психиатром, в результате чего лечение становится бесполезным.
Как следствие всех вышеперечисленных факторов, пациент с функциональными расстройствами часто ощущает себя “проваливающимся в пропасть медицины”.
Около 100 лет назад неврологи и психиатры полагали, что эти симптомы являются результатом нарушения функций нервной системы, а психологические факторы, несмотря на свою значимость, могут отсутствовать.
Изучая проблемы диагностики и лечения функциональных расстройств, неврологи написали книги о «функциональных нервных расстройствах», руководствуясь здравым смыслом. И наконец-то «колесо» вновь стало возвращаться назад к прежней точке зрения. На наш взгляд трудности в этой области можно было бы преодолеть посредством лучшего образования медицинских работников в вопросах диагностики и лечения этих расстройств.
Вы можете прочитать обзорную статьи, которую Джон Стоун написал для врачей, нажав по ссылке справа.
ПОМНИТЕ, ВАШИ СИМПТОМЫ РЕАЛЬНЫ, ЕСЛИ ДАЖЕ ВРАЧИ ИЛИ КТО-ТО ДРУГОЙ ПЫТАЕТСЯ УБЕДИТЬ ВАС, ЧТО ИХ НЕТ!


We will be re-directing you to the University of Edinburgh’s donate page, which enable donations in a secure manner on our behalf. We use donations for keeping the site running and further FND research.
