FND means functional neurological disorder. It describes a problem with the function of the nervous system – a software problem rather than a hardware problem. In recent years though several studies have suggested that people with FND may have some changes to the structure of their brain too. Is this correct? And if so what does it mean for how we think about FND?
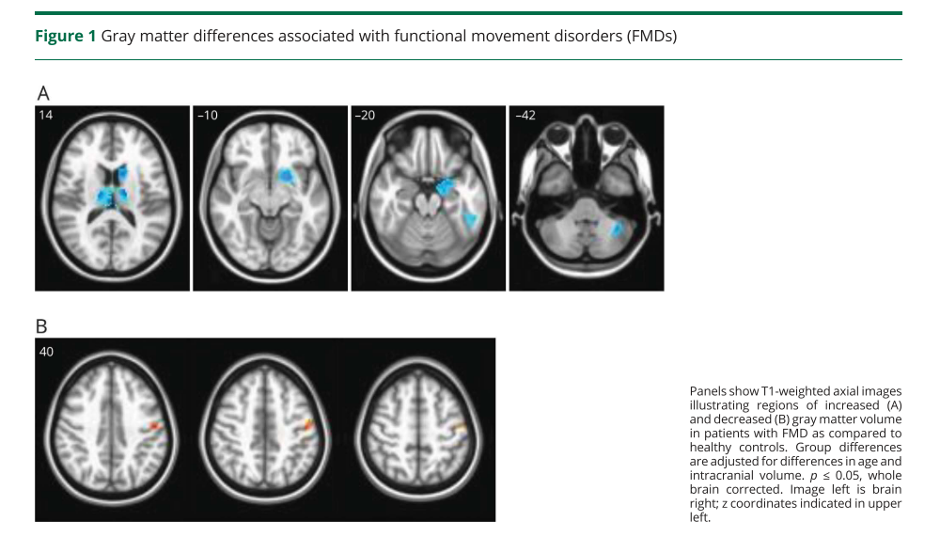
There have been several interesting studies of differences in brain structure between FND and healthy controls. In one study Carine Maurer in the US and colleagues compared brain scans of 48 people with FND movement disorders with 55 healthy controls of the same age and gender1.
They found that there were some areas of the brain, in the ‘Gray’ matter that were smaller in patients with FND than healthy controls. These were particularly in areas of the brain related to movement and sensation and areas that are important in experiencing emotions and ‘fight or flight’ responses.
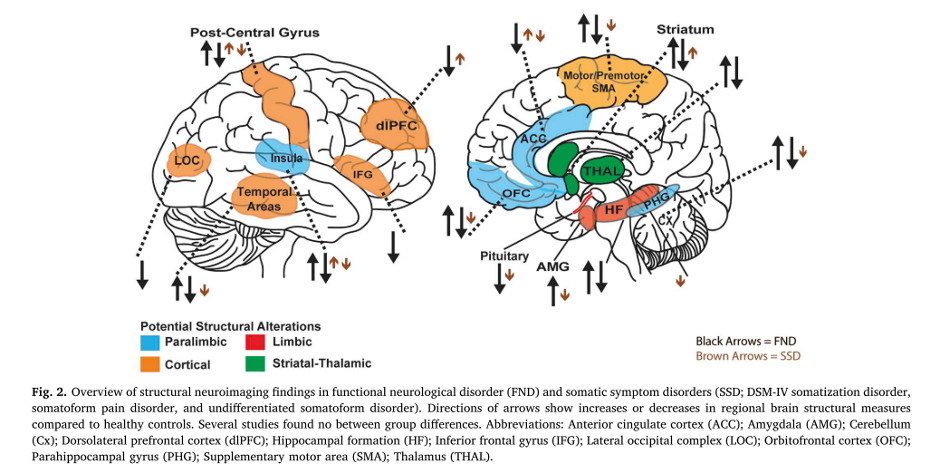
Several other studies have shown somewhat different findings. I was a co-author on a paper led by David Perez and Indrit Begue, that summarised those findings2. A consistent pattern hasn’t emerged but it seems likely that there are differences, at a group level between patients who have FND and healthy individuals.
The changes being reported are all subtle and at a group level, so needs the pooling of the scans of lots of individuals to find a discernible difference. The approach taken to investigate these potential brain changes are using research methods that are not validated for clinical use and the clinical significance of these findings remains poorly understood. Furthermore, they are not detectable on individual brain scans which are typically normal in FND, unless the person has another neurological condition or an incidental finding (those are common occurring in 1 in 6 of the population)3
We don’t know. It could be that people with FND are born with differently structured brains that make them susceptible to the condition.
Our brains are constantly changing, developing and shrinking throughout our life. It’s a bit like a muscle. If you use a certain part a lot then it will get bigger, if you don’t it may shrink. For example, London Taxi Drivers who had to learn all the streets of London by heart, have a larger ‘navigational’ area of the brain than people who are not taxi drivers1.
In fact, people with most psychiatric disorders, such as depression, anxiety and PTSD, have also been found to have structural changes in their brain too, and to a degree that is similar to the studies in FND.
The structural ‘hardware’ changes may be important because these findings might promote the vulnerability in the system to frequent ‘software crashes’. The structural alterations being generally found in cortical and limbic areas that are communicating with sensorimotor pathways.
Another possibility is that people with FND develop changes in the structure of the brain as a consequence of having the condition, rather than a cause of the condition. That certainly happens in other neurological conditions.
It seems likely that the answer will lie somewhere in between. There probably are structural vulnerabilities and the condition probably changes the brain too.
FND has a really difficult and stigmatised history. For a very long time it was classified as a purely psychological disorder. In the last 20 years we have been uncovering some of the ways in which FND symptoms are caused in the brain, and have made a lot of progress, but we are still a long way from a definite model.
All of this shakes up our preconceived ideas about what a neurological disorder is and what a psychiatric disorder is. It turns out that the division is false and all of them are occurring in the brain.
The name Functional Neurological Disorder describes a condition in which there is a disorder of nervous system functioning. It’s called that in large part because of the way that it is diagnosed. For example:
All of these common clinical features clearly show there is a problem with function which is much more obvious than a subtle problem with structure. If it was the structure then the weakness would not transiently improve, the tremor would not transiently stop, and the gait would not improve.
From a practical point of view, understanding what these clinical features mean can really help people with FND to see that there is a potential for recovery, that their situation and symptoms may not be as irreversible as they may first appear.
The physiotherapy and psychological therapies being developed for FND help people to get their heads round these issues and build on them for treatment to help ‘retrain the brain’.
In physiotherapy, if someone’s walking can improve when they are going fast, the physio may use that to regain more normal ‘automatic’ walking patterns. In psychological therapy, understanding more about how weird the brain is, and how working too hard to make a movement actually make its worse, and more so if you get frustrated or worried, can help.
Many people with FND can’t improve, even when they understand the condition and are really motivated to change. Perhaps the structural changes we have found, or the changes in brain function are too difficult to overcome. We just don’t know at this point whether that is the case or not.
Most people with FND think, at some point, that there must be some damage to their brain to cause the symptoms they have.
Understanding how symptoms can transiently improve and how rehabilitation therapies can build on then to gradually gain greater improvement is a key part of clinical treatment. These new FND treatments have already been shown to be promising in randomised controlled clinical trials.
We may at some stage need to build in an understanding of these structural changes into our models and the way we explain FND. But at the moment we simply don’t have enough data to be able to use this information in a clinically useful way.
If the structural changes have always been there, then that’s clearly important but we still don’t know if they represent an obstacle to improvement.
If the structural changes happen because of the condition, then we need to help patients understand that FND has changed their brain, but treatment can hopefully change it back again.
References


We will be re-directing you to the University of Edinburgh’s donate page, which enable donations in a secure manner on our behalf. We use donations for keeping the site running and further FND research.
